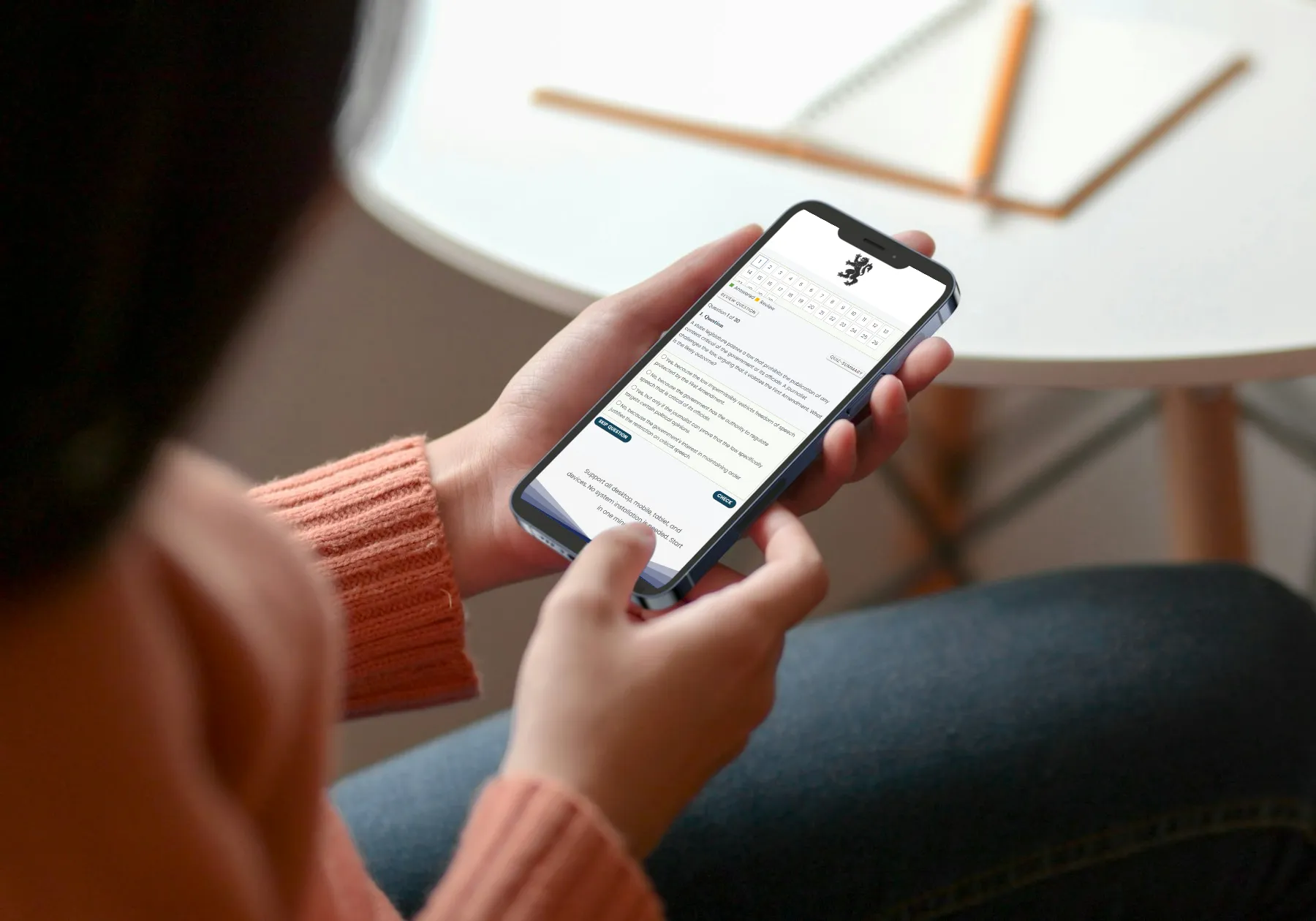
Quiz-summary
0 of 29 questions completed
Questions:
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
Information
Premium Practice Questions
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading...
You must sign in or sign up to start the quiz.
You have to finish following quiz, to start this quiz:
Results
0 of 29 questions answered correctly
Your time:
Time has elapsed
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- Answered
- Review
-
Question 1 of 29
1. Question
The evaluation methodology shows that during a routine morning check at a community health center in a provincial district, the pharmacist discovers that the vaccine refrigerator thermometer indicates a temperature of 14 degrees Celsius due to a localized power interruption that occurred overnight. Several parents are already waiting with their children for their scheduled measles and pentavalent vaccine doses. The facility manager pressures the pharmacist to proceed with the vaccination to avoid wasting the doses and to maintain the facilitys high immunization coverage rates. According to Philippine regulatory standards for cold chain management, which course of action must the pharmacist take to fulfill their professional and legal obligations?
Correct
Correct: Quarantining the affected vaccines immediately, documenting the duration and temperature of the excursion, and contacting the manufacturer or the Department of Health for stability data before further use is the required protocol. Under Philippine Department of Health Administrative Order No. 2020-0017, any break in the cold chain necessitates the isolation of products to prevent accidental use until their potency is verified through official stability studies or manufacturer guidance. This aligns with the Philippine Pharmacy Act (RA 10918), which mandates that pharmacists ensure the safety and efficacy of all pharmaceutical products dispensed.
Incorrect: Relying on a visual inspection for physical changes like turbidity is insufficient because many vaccines lose potency due to heat or freeze damage without any visible alteration. Prioritizing administration based on patient travel distance ignores the risk of providing a sub-therapeutic dose. Attempting to compensate for heat exposure by lowering the refrigerator temperature within the 2-8 degrees Celsius range is not a recognized scientific method and increases the risk of freezing freeze-sensitive vaccines like DTP or HepB. Proceeding with immunization while planning for retrospective monitoring of adverse reactions is ethically unacceptable, as the primary risk of cold chain failure is the failure to provide immunity, leaving the population vulnerable to vaccine-preventable diseases.
Takeaway: Any deviation from the required 2 to 8 degrees Celsius storage range requires immediate quarantine and professional verification of stability to ensure patient safety and vaccine efficacy.
Incorrect
Correct: Quarantining the affected vaccines immediately, documenting the duration and temperature of the excursion, and contacting the manufacturer or the Department of Health for stability data before further use is the required protocol. Under Philippine Department of Health Administrative Order No. 2020-0017, any break in the cold chain necessitates the isolation of products to prevent accidental use until their potency is verified through official stability studies or manufacturer guidance. This aligns with the Philippine Pharmacy Act (RA 10918), which mandates that pharmacists ensure the safety and efficacy of all pharmaceutical products dispensed.
Incorrect: Relying on a visual inspection for physical changes like turbidity is insufficient because many vaccines lose potency due to heat or freeze damage without any visible alteration. Prioritizing administration based on patient travel distance ignores the risk of providing a sub-therapeutic dose. Attempting to compensate for heat exposure by lowering the refrigerator temperature within the 2-8 degrees Celsius range is not a recognized scientific method and increases the risk of freezing freeze-sensitive vaccines like DTP or HepB. Proceeding with immunization while planning for retrospective monitoring of adverse reactions is ethically unacceptable, as the primary risk of cold chain failure is the failure to provide immunity, leaving the population vulnerable to vaccine-preventable diseases.
Takeaway: Any deviation from the required 2 to 8 degrees Celsius storage range requires immediate quarantine and professional verification of stability to ensure patient safety and vaccine efficacy.
-
Question 2 of 29
2. Question
The performance metrics show a growing trend of community pharmacists in the Philippines participating as sub-investigators in multi-center clinical trials. When enrolling a patient into a new study regarding a novel antihypertensive agent, which of the following actions most accurately reflects the regulatory requirements for informed consent as mandated by the Philippine Health Research Ethics Board (PHREB) and the National Ethical Guidelines?
Correct
Correct: Ensuring the participant receives a full explanation of the study’s nature and signs a written consent form approved by an accredited Ethics Review Committee prior to any intervention. According to the National Ethical Guidelines for Health and Health-Related Research and the Philippine Health Research Ethics Board (PHREB), informed consent is a mandatory process where the participant must be fully informed of the study’s purpose, risks, and benefits. This process must be documented through a written form that has been pre-approved by an accredited Ethics Review Committee (ERC) to ensure the protection of human subjects before any research activities commence.
Incorrect: Relying on verbal consent witnessed by a professional colleague fails to meet the legal documentation standards required for clinical trials in the Philippines, which necessitate a signed written record. Providing only a summary of benefits while including a liability waiver is a violation of ethical standards, as informed consent documents must not contain language that causes the participant to waive legal rights or releases the researcher from liability for negligence. Initiating trial phases while documentation is still pending approval is a significant regulatory breach, as no research-related procedures may be performed on a human subject until both the ERC has granted approval and the subject has provided formal consent.
Takeaway: Valid informed consent in Philippine pharmacy research requires a written, ERC-approved document signed by the participant before any study-related procedures are initiated.
Incorrect
Correct: Ensuring the participant receives a full explanation of the study’s nature and signs a written consent form approved by an accredited Ethics Review Committee prior to any intervention. According to the National Ethical Guidelines for Health and Health-Related Research and the Philippine Health Research Ethics Board (PHREB), informed consent is a mandatory process where the participant must be fully informed of the study’s purpose, risks, and benefits. This process must be documented through a written form that has been pre-approved by an accredited Ethics Review Committee (ERC) to ensure the protection of human subjects before any research activities commence.
Incorrect: Relying on verbal consent witnessed by a professional colleague fails to meet the legal documentation standards required for clinical trials in the Philippines, which necessitate a signed written record. Providing only a summary of benefits while including a liability waiver is a violation of ethical standards, as informed consent documents must not contain language that causes the participant to waive legal rights or releases the researcher from liability for negligence. Initiating trial phases while documentation is still pending approval is a significant regulatory breach, as no research-related procedures may be performed on a human subject until both the ERC has granted approval and the subject has provided formal consent.
Takeaway: Valid informed consent in Philippine pharmacy research requires a written, ERC-approved document signed by the participant before any study-related procedures are initiated.
-
Question 3 of 29
3. Question
The performance metrics show that a newly established community pharmacy is organizing its regulatory calendar to ensure strict adherence to the Comprehensive Dangerous Drugs Act of 2002. To maintain compliance with the Philippine Drug Enforcement Agency (PDEA) regarding the monitoring of controlled substances, which protocol must the supervising pharmacist implement for the submission of transaction reports?
Correct
Correct: Under Republic Act No. 9165, also known as the Comprehensive Dangerous Drugs Act of 2002, and its associated regulations, retail pharmacies holding an S2 license are mandated to submit a semi-annual report of all transactions involving dangerous drugs. These reports must be filed with the Philippine Drug Enforcement Agency (PDEA) within the first fifteen days of January and July of each year, covering the transactions from the previous six-month period. This regulatory requirement is crucial for the monitoring and prevention of the diversion of controlled substances into illicit channels.
Incorrect: Maintaining a local record for two years and submitting quarterly summaries is incorrect because the statutory reporting frequency for dangerous drug transactions to the PDEA is semi-annual rather than quarterly. Filing monthly electronic reports within ten days of the following month is not the standard reporting period prescribed for general retail pharmacies under the current implementing rules and regulations of RA 9165. Submitting an annual inventory report every December is insufficient as it fails to comply with the mandatory twice-yearly reporting schedule and the specific fifteen-day submission window required by the regulatory framework.
Takeaway: Licensed pharmacists must ensure the submission of semi-annual dangerous drug transaction reports to the PDEA within the first fifteen days of January and July.
Incorrect
Correct: Under Republic Act No. 9165, also known as the Comprehensive Dangerous Drugs Act of 2002, and its associated regulations, retail pharmacies holding an S2 license are mandated to submit a semi-annual report of all transactions involving dangerous drugs. These reports must be filed with the Philippine Drug Enforcement Agency (PDEA) within the first fifteen days of January and July of each year, covering the transactions from the previous six-month period. This regulatory requirement is crucial for the monitoring and prevention of the diversion of controlled substances into illicit channels.
Incorrect: Maintaining a local record for two years and submitting quarterly summaries is incorrect because the statutory reporting frequency for dangerous drug transactions to the PDEA is semi-annual rather than quarterly. Filing monthly electronic reports within ten days of the following month is not the standard reporting period prescribed for general retail pharmacies under the current implementing rules and regulations of RA 9165. Submitting an annual inventory report every December is insufficient as it fails to comply with the mandatory twice-yearly reporting schedule and the specific fifteen-day submission window required by the regulatory framework.
Takeaway: Licensed pharmacists must ensure the submission of semi-annual dangerous drug transaction reports to the PDEA within the first fifteen days of January and July.
-
Question 4 of 29
4. Question
The monitoring system demonstrates a significant gap in the local community’s understanding of the National Immunization Program and the risks of antimicrobial resistance. According to the Philippine Pharmacy Act (RA 10918) and the Universal Health Care Act (RA 11223), which approach should the community pharmacist prioritize when implementing a health promotion campaign?
Correct
Correct: Collaborating with the local health office to provide evidence-based counseling and educational materials that align with Department of Health (DOH) public health goals ensures compliance with RA 10918 and the Universal Health Care Act by prioritizing national health priorities and primary care.
Incorrect: Developing independent health brochures focused on high-demand supplements prioritizes commercial interests over the mandated public health roles defined in the Philippine Pharmacy Act. Distributing prescription-only medication samples during screening programs violates regulatory standards regarding the dispensing of restricted drugs and patient safety. Focusing exclusively on digital marketing for over-the-counter medications fails to provide the comprehensive, evidence-based education required for programs like the National Immunization Program.
Takeaway: Community pharmacists in the Philippines are legally mandated to align health promotion activities with Department of Health standards to ensure public safety and consistency in health education.
Incorrect
Correct: Collaborating with the local health office to provide evidence-based counseling and educational materials that align with Department of Health (DOH) public health goals ensures compliance with RA 10918 and the Universal Health Care Act by prioritizing national health priorities and primary care.
Incorrect: Developing independent health brochures focused on high-demand supplements prioritizes commercial interests over the mandated public health roles defined in the Philippine Pharmacy Act. Distributing prescription-only medication samples during screening programs violates regulatory standards regarding the dispensing of restricted drugs and patient safety. Focusing exclusively on digital marketing for over-the-counter medications fails to provide the comprehensive, evidence-based education required for programs like the National Immunization Program.
Takeaway: Community pharmacists in the Philippines are legally mandated to align health promotion activities with Department of Health standards to ensure public safety and consistency in health education.
-
Question 5 of 29
5. Question
The performance metrics show that a community pharmacy in Manila has a high rate of expired medications being pulled from the shelves during monthly inventory audits. To align the pharmacy operations with the Philippine FDA Manual of Burden for Good Distribution and Storage Practices, which inventory management strategy should the pharmacist-in-charge implement to ensure regulatory compliance and patient safety?
Correct
Correct: Prioritize the distribution of products with the earliest expiration dates regardless of when they were received into the inventory system. This approach follows the First-Expiry First-Out (FEFO) principle, which is the standard requirement under the Philippine Food and Drug Administration (FDA) guidelines for Good Storage and Distribution Practices. By focusing on the expiration date rather than the arrival date, the pharmacist ensures that medications are dispensed before they lose potency or become unsafe, directly complying with the quality assurance mandates of Republic Act No. 10918.
Incorrect: Prioritizing distribution based on the sequence of arrival (First-In First-Out or FIFO) is a common inventory error in pharmacy because a newer shipment may occasionally have an earlier expiration date than stock already on the shelf. Prioritizing products with the longest shelf life is an incorrect practice that leads to the accumulation of near-expiry drugs, increasing the risk of dispensing expired medication to the public. Using the date of manufacture as the primary driver for rotation is insufficient because it does not account for the specific stability data and expiration limits established by the manufacturer and approved by the FDA.
Takeaway: Under Philippine regulatory standards, the FEFO principle must take precedence over FIFO to ensure patient safety and minimize the wastage of pharmaceutical products.
Incorrect
Correct: Prioritize the distribution of products with the earliest expiration dates regardless of when they were received into the inventory system. This approach follows the First-Expiry First-Out (FEFO) principle, which is the standard requirement under the Philippine Food and Drug Administration (FDA) guidelines for Good Storage and Distribution Practices. By focusing on the expiration date rather than the arrival date, the pharmacist ensures that medications are dispensed before they lose potency or become unsafe, directly complying with the quality assurance mandates of Republic Act No. 10918.
Incorrect: Prioritizing distribution based on the sequence of arrival (First-In First-Out or FIFO) is a common inventory error in pharmacy because a newer shipment may occasionally have an earlier expiration date than stock already on the shelf. Prioritizing products with the longest shelf life is an incorrect practice that leads to the accumulation of near-expiry drugs, increasing the risk of dispensing expired medication to the public. Using the date of manufacture as the primary driver for rotation is insufficient because it does not account for the specific stability data and expiration limits established by the manufacturer and approved by the FDA.
Takeaway: Under Philippine regulatory standards, the FEFO principle must take precedence over FIFO to ensure patient safety and minimize the wastage of pharmaceutical products.
-
Question 6 of 29
6. Question
Which approach would be most consistent with the Code of Ethics for Philippine Pharmacists and the Data Privacy Act of 2012 when a pharmacist intends to share a unique clinical case on a professional social media platform for educational purposes?
Correct
Correct: Removing all direct and indirect identifiers as mandated by the Data Privacy Act of 2012 (RA 10173) and the Code of Ethics for Philippine Pharmacists ensures that patient anonymity is preserved. Under Philippine law, sensitive personal information requires stringent protection, and professional ethics dictate that any public or semi-public sharing of clinical data must be done in a manner that prevents any possibility of the patient being identified, even through the combination of various data points.
Incorrect: Sharing clinical information in closed groups while only redacting names and birthdates is insufficient because other identifiers, such as unique medical conditions or specific combinations of medications, can still lead to jigsaw identification. Relying on verbal consent is legally inadequate under the Data Privacy Act for the processing of sensitive health information for public or digital dissemination. Limiting a post to clinical findings while only excluding location and date does not meet the comprehensive de-identification standards required to protect patient rights and maintain professional standards in the Philippines.
Takeaway: Philippine pharmacists must prioritize absolute de-identification and adhere to the Data Privacy Act of 2012 when utilizing social media for professional education to ensure patient confidentiality is never compromised.
Incorrect
Correct: Removing all direct and indirect identifiers as mandated by the Data Privacy Act of 2012 (RA 10173) and the Code of Ethics for Philippine Pharmacists ensures that patient anonymity is preserved. Under Philippine law, sensitive personal information requires stringent protection, and professional ethics dictate that any public or semi-public sharing of clinical data must be done in a manner that prevents any possibility of the patient being identified, even through the combination of various data points.
Incorrect: Sharing clinical information in closed groups while only redacting names and birthdates is insufficient because other identifiers, such as unique medical conditions or specific combinations of medications, can still lead to jigsaw identification. Relying on verbal consent is legally inadequate under the Data Privacy Act for the processing of sensitive health information for public or digital dissemination. Limiting a post to clinical findings while only excluding location and date does not meet the comprehensive de-identification standards required to protect patient rights and maintain professional standards in the Philippines.
Takeaway: Philippine pharmacists must prioritize absolute de-identification and adhere to the Data Privacy Act of 2012 when utilizing social media for professional education to ensure patient confidentiality is never compromised.
-
Question 7 of 29
7. Question
Strategic planning requires a robust validation protocol for terminal sterilization in pharmaceutical manufacturing to ensure patient safety and compliance with Philippine FDA standards and PIC/S GMP guidelines. Which of the following approaches represents the most rigorous and standard method for validating a steam sterilization cycle to ensure a Sterility Assurance Level of 10 to the power of negative 6?
Correct
Correct: Implementing an overkill approach using a biological indicator like Geobacillus stearothermophilus to achieve a 12-log reduction of a resistant microorganism. This method is the gold standard in Philippine FDA-regulated manufacturing environments following PIC/S GMP guidelines. It ensures a Sterility Assurance Level (SAL) of 10 to the power of negative 6 by proving the cycle can destroy a high concentration of the most heat-resistant spores, providing a significant safety margin over the actual bioburden.
Incorrect: Relying primarily on calibrated physical parameters such as temperature and pressure sensors is insufficient because these instruments only measure the environment and do not confirm biological lethality within the load. Utilizing a bioburden-based approach that targets the destruction of the most frequent environmental isolates is inadequate as it fails to account for the most resistant microbial strains that might be present in lower numbers. Validating the efficacy of the sterilization process based on the consistent color change of chemical indicators is a common misconception; chemical indicators are process indicators used for routine monitoring to distinguish processed from unprocessed items, but they do not provide the quantitative data required for cycle validation.
Takeaway: Sterilization validation must utilize biological indicators to confirm a Sterility Assurance Level that guarantees the destruction of the most resistant microbial forms.
Incorrect
Correct: Implementing an overkill approach using a biological indicator like Geobacillus stearothermophilus to achieve a 12-log reduction of a resistant microorganism. This method is the gold standard in Philippine FDA-regulated manufacturing environments following PIC/S GMP guidelines. It ensures a Sterility Assurance Level (SAL) of 10 to the power of negative 6 by proving the cycle can destroy a high concentration of the most heat-resistant spores, providing a significant safety margin over the actual bioburden.
Incorrect: Relying primarily on calibrated physical parameters such as temperature and pressure sensors is insufficient because these instruments only measure the environment and do not confirm biological lethality within the load. Utilizing a bioburden-based approach that targets the destruction of the most frequent environmental isolates is inadequate as it fails to account for the most resistant microbial strains that might be present in lower numbers. Validating the efficacy of the sterilization process based on the consistent color change of chemical indicators is a common misconception; chemical indicators are process indicators used for routine monitoring to distinguish processed from unprocessed items, but they do not provide the quantitative data required for cycle validation.
Takeaway: Sterilization validation must utilize biological indicators to confirm a Sterility Assurance Level that guarantees the destruction of the most resistant microbial forms.
-
Question 8 of 29
8. Question
When evaluating the standard operating procedures for dispensing medications in a community pharmacy setting in the Philippines, which protocol most effectively minimizes the risk of medication errors related to patient misidentification?
Correct
Correct: In accordance with the Philippine Pharmacy Act (Republic Act No. 10918) and the Department of Health guidelines on patient safety, pharmacists are required to ensure the right drug is dispensed to the right patient. The most effective protocol involves using at least two unique patient identifiers, such as the full name and date of birth. Requiring the patient or their representative to actively state this information, rather than the pharmacist providing it for confirmation, prevents errors associated with passive recognition or patients mishearing a name in a busy environment. Cross-referencing this verbal data with both the physical prescription and the pharmacy electronic record provides a multi-layered verification process.
Incorrect: Verifying identity by calling out a name and waiting for a nod or a yes is considered a passive identification technique. This is prone to error because patients may be distracted, have hearing impairments, or simply assume they are being called if their name is similar to another. Using the medication name as an identifier is fundamentally flawed because the drug name identifies the treatment, not the individual receiving it. Relying exclusively on matching a prescription number or claim stub to a label is an administrative check that does not account for the possibility of the wrong stub being handed to a patient or a clerical error during the intake process; it lacks the necessary direct human verification of the patient identity.
Takeaway: Active verification using two unique identifiers is the essential standard for preventing patient misidentification in Philippine pharmacy practice.
Incorrect
Correct: In accordance with the Philippine Pharmacy Act (Republic Act No. 10918) and the Department of Health guidelines on patient safety, pharmacists are required to ensure the right drug is dispensed to the right patient. The most effective protocol involves using at least two unique patient identifiers, such as the full name and date of birth. Requiring the patient or their representative to actively state this information, rather than the pharmacist providing it for confirmation, prevents errors associated with passive recognition or patients mishearing a name in a busy environment. Cross-referencing this verbal data with both the physical prescription and the pharmacy electronic record provides a multi-layered verification process.
Incorrect: Verifying identity by calling out a name and waiting for a nod or a yes is considered a passive identification technique. This is prone to error because patients may be distracted, have hearing impairments, or simply assume they are being called if their name is similar to another. Using the medication name as an identifier is fundamentally flawed because the drug name identifies the treatment, not the individual receiving it. Relying exclusively on matching a prescription number or claim stub to a label is an administrative check that does not account for the possibility of the wrong stub being handed to a patient or a clerical error during the intake process; it lacks the necessary direct human verification of the patient identity.
Takeaway: Active verification using two unique identifiers is the essential standard for preventing patient misidentification in Philippine pharmacy practice.
-
Question 9 of 29
9. Question
Strategic planning requires a clinical pharmacist in a Philippine hospital setting to perform comprehensive medication therapy management for patients with fluctuating physiological parameters. When reviewing a patient’s clinical laboratory results that show an increase in serum creatinine, which professional approach should the pharmacist take to ensure appropriate dose adjustment for a renally cleared medication according to the standards of practice in the Philippines?
Correct
Correct: Evaluating the patient’s serum creatinine levels in conjunction with age, weight, and gender to estimate the glomerular filtration rate before recommending a dosage reduction for a renally cleared antimicrobial. This approach aligns with the Philippine Pharmacy Act (RA 10918), which defines clinical pharmacy services as including the monitoring of drug utilization and the provision of medication therapy management. Since serum creatinine is a product of muscle metabolism, it must be integrated into equations like Cockcroft-Gault to provide a reliable estimate of renal clearance for accurate dose adjustment, rather than using the raw laboratory value in isolation.
Incorrect: Relying solely on the reported serum creatinine concentration as the primary indicator is insufficient because it does not account for the patient’s muscle mass or age, which can lead to significant dosing errors and potential toxicity or subtherapeutic dosing. Delaying the initiation of the prescribed maintenance dose until a repeat laboratory test confirms the result is often clinically inappropriate in acute settings and may lead to treatment failure or worsening of the patient’s condition. Utilizing blood urea nitrogen levels as the definitive clinical marker is unreliable for dose adjustment because BUN is influenced by non-renal factors such as diet, hydration status, and gastrointestinal bleeding.
Takeaway: Effective dose adjustment requires the synthesis of laboratory data with patient-specific physiological factors to accurately estimate organ function and optimize therapeutic outcomes.
Incorrect
Correct: Evaluating the patient’s serum creatinine levels in conjunction with age, weight, and gender to estimate the glomerular filtration rate before recommending a dosage reduction for a renally cleared antimicrobial. This approach aligns with the Philippine Pharmacy Act (RA 10918), which defines clinical pharmacy services as including the monitoring of drug utilization and the provision of medication therapy management. Since serum creatinine is a product of muscle metabolism, it must be integrated into equations like Cockcroft-Gault to provide a reliable estimate of renal clearance for accurate dose adjustment, rather than using the raw laboratory value in isolation.
Incorrect: Relying solely on the reported serum creatinine concentration as the primary indicator is insufficient because it does not account for the patient’s muscle mass or age, which can lead to significant dosing errors and potential toxicity or subtherapeutic dosing. Delaying the initiation of the prescribed maintenance dose until a repeat laboratory test confirms the result is often clinically inappropriate in acute settings and may lead to treatment failure or worsening of the patient’s condition. Utilizing blood urea nitrogen levels as the definitive clinical marker is unreliable for dose adjustment because BUN is influenced by non-renal factors such as diet, hydration status, and gastrointestinal bleeding.
Takeaway: Effective dose adjustment requires the synthesis of laboratory data with patient-specific physiological factors to accurately estimate organ function and optimize therapeutic outcomes.
-
Question 10 of 29
10. Question
The audit findings indicate that a community pharmacy in the Philippines has experienced a significant increase in near-miss medication errors involving look-alike, sound-alike (LASA) medications over the last six months. In accordance with the Philippine Pharmacy Act and the principles of Good Pharmacy Practice (GPP), which risk management strategy should the pharmacist-in-charge implement to most effectively minimize the risk of future dispensing errors?
Correct
Correct: Establishing a voluntary, non-punitive incident reporting framework that utilizes Root Cause Analysis (RCA) to identify and rectify latent systemic vulnerabilities. This approach is consistent with the Philippine Pharmacy Act (RA 10918) and Good Pharmacy Practice (GPP) standards, which emphasize the pharmacist’s role in patient safety. By fostering a Just Culture, the pharmacy encourages the reporting of near-misses and errors without fear of retribution, allowing the organization to identify and fix the underlying process flaws—such as poor lighting, look-alike packaging, or workflow interruptions—that lead to mistakes.
Incorrect: Implementing a performance-based incentive program that rewards staff members who maintain zero recorded errors during their scheduled shifts is counterproductive. This often leads to the suppression of error reporting and creates a false sense of security, as staff may hide mistakes to protect their rewards. Mandating that all high-alert and LASA medications be stored in a centralized, locked cabinet accessible only by the pharmacist-on-duty is a restrictive measure that may create operational bottlenecks and does not address the cognitive nature of selection errors. Increasing the frequency of internal quality audits from quarterly to monthly is a monitoring strategy but lacks the proactive, analytical depth required to redesign unsafe processes or address the root causes of clinical risks.
Takeaway: Sustainable risk management in pharmacy operations relies on a non-punitive culture that prioritizes systemic analysis over individual blame to prevent the recurrence of medication errors.
Incorrect
Correct: Establishing a voluntary, non-punitive incident reporting framework that utilizes Root Cause Analysis (RCA) to identify and rectify latent systemic vulnerabilities. This approach is consistent with the Philippine Pharmacy Act (RA 10918) and Good Pharmacy Practice (GPP) standards, which emphasize the pharmacist’s role in patient safety. By fostering a Just Culture, the pharmacy encourages the reporting of near-misses and errors without fear of retribution, allowing the organization to identify and fix the underlying process flaws—such as poor lighting, look-alike packaging, or workflow interruptions—that lead to mistakes.
Incorrect: Implementing a performance-based incentive program that rewards staff members who maintain zero recorded errors during their scheduled shifts is counterproductive. This often leads to the suppression of error reporting and creates a false sense of security, as staff may hide mistakes to protect their rewards. Mandating that all high-alert and LASA medications be stored in a centralized, locked cabinet accessible only by the pharmacist-on-duty is a restrictive measure that may create operational bottlenecks and does not address the cognitive nature of selection errors. Increasing the frequency of internal quality audits from quarterly to monthly is a monitoring strategy but lacks the proactive, analytical depth required to redesign unsafe processes or address the root causes of clinical risks.
Takeaway: Sustainable risk management in pharmacy operations relies on a non-punitive culture that prioritizes systemic analysis over individual blame to prevent the recurrence of medication errors.
-
Question 11 of 29
11. Question
To address the challenge of managing pharmaceutical waste and maintaining inventory integrity, which procedure should a supervising pharmacist in the Philippines implement when handling products that have reached their expiration date or sustained packaging damage?
Correct
Correct: Under the Philippine Pharmacy Act (RA 10918) and FDA Good Distribution Practices, expired or damaged products must be physically segregated from saleable stock in a designated, clearly labeled area to prevent accidental dispensing. Proper documentation, including batch numbers and expiry dates, is essential for traceability and regulatory compliance. Following the distributor’s Return Goods Authorization (RGA) process ensures that the chain of custody is maintained and that the pharmacy receives appropriate credit while complying with national disposal standards.
Incorrect: Returning items immediately without prior notification or an RGA often leads to logistical errors and violates standard distributor agreements that require specific documentation for tracking and credit verification. Keeping expired items on the dispensing shelf, even if marked with stickers, increases the risk of medication errors and violates FDA requirements for strict physical segregation of non-conforming products. Local disposal without distributor involvement bypasses the necessary verification process for credit and may not comply with specific FDA and DENR requirements for the disposal of pharmaceutical waste which often require manufacturer oversight.
Takeaway: Effective inventory management in Philippine pharmacies requires strict physical segregation of expired goods and adherence to formal distributor return protocols to ensure regulatory compliance and patient safety.
Incorrect
Correct: Under the Philippine Pharmacy Act (RA 10918) and FDA Good Distribution Practices, expired or damaged products must be physically segregated from saleable stock in a designated, clearly labeled area to prevent accidental dispensing. Proper documentation, including batch numbers and expiry dates, is essential for traceability and regulatory compliance. Following the distributor’s Return Goods Authorization (RGA) process ensures that the chain of custody is maintained and that the pharmacy receives appropriate credit while complying with national disposal standards.
Incorrect: Returning items immediately without prior notification or an RGA often leads to logistical errors and violates standard distributor agreements that require specific documentation for tracking and credit verification. Keeping expired items on the dispensing shelf, even if marked with stickers, increases the risk of medication errors and violates FDA requirements for strict physical segregation of non-conforming products. Local disposal without distributor involvement bypasses the necessary verification process for credit and may not comply with specific FDA and DENR requirements for the disposal of pharmaceutical waste which often require manufacturer oversight.
Takeaway: Effective inventory management in Philippine pharmacies requires strict physical segregation of expired goods and adherence to formal distributor return protocols to ensure regulatory compliance and patient safety.
-
Question 12 of 29
12. Question
Assessment of the regulatory criteria used by the Dangerous Drugs Board (DDB) in the Philippines to categorize a psychotropic substance under Schedule I reveals that which of the following best defines the requirements for this classification?
Correct
Correct: Under the regulatory framework of the Philippine Dangerous Drugs Board (DDB) and the Comprehensive Dangerous Drugs Act of 2002 (RA 9165), substances classified under Schedule I are those determined to have a very high potential for abuse, pose a particularly serious threat to public health, and have very little or no currently accepted therapeutic value in medical practice. This classification necessitates the most stringent level of control and prohibition of use outside of strictly regulated scientific research.
Incorrect: Identifying substances with high abuse potential but established therapeutic benefits describes the criteria for Schedule II, where medical utility is recognized despite the risk of dependence. Focusing on substances used in the manufacture of essential precursor chemicals is incorrect because precursors and essential chemicals are categorized under separate lists (Table I and Table II of the 1988 UN Convention) rather than the standard drug schedules I-IV. Classifying substances as low-risk items available over-the-counter describes the characteristics of Schedule V or non-controlled substances, which contradicts the high-risk profile required for a Schedule I designation.
Takeaway: Schedule I substances are defined by their lack of recognized medical use and high potential for abuse, requiring the highest level of regulatory restriction under Philippine law.
Incorrect
Correct: Under the regulatory framework of the Philippine Dangerous Drugs Board (DDB) and the Comprehensive Dangerous Drugs Act of 2002 (RA 9165), substances classified under Schedule I are those determined to have a very high potential for abuse, pose a particularly serious threat to public health, and have very little or no currently accepted therapeutic value in medical practice. This classification necessitates the most stringent level of control and prohibition of use outside of strictly regulated scientific research.
Incorrect: Identifying substances with high abuse potential but established therapeutic benefits describes the criteria for Schedule II, where medical utility is recognized despite the risk of dependence. Focusing on substances used in the manufacture of essential precursor chemicals is incorrect because precursors and essential chemicals are categorized under separate lists (Table I and Table II of the 1988 UN Convention) rather than the standard drug schedules I-IV. Classifying substances as low-risk items available over-the-counter describes the characteristics of Schedule V or non-controlled substances, which contradicts the high-risk profile required for a Schedule I designation.
Takeaway: Schedule I substances are defined by their lack of recognized medical use and high potential for abuse, requiring the highest level of regulatory restriction under Philippine law.
-
Question 13 of 29
13. Question
During the evaluation of a patient’s long-term prescription for hypertension at a community pharmacy in Quezon City, the patient mentions they may stop taking the medication because the prescribed innovator brand is too expensive for their fixed income. Which action by the pharmacist best demonstrates professional advocacy for patient rights and access to essential medicines within the Philippine regulatory framework?
Correct
Correct: Under Republic Act No. 6675, also known as the Generics Act of 1988, and Republic Act No. 9502, the Universally Accessible Cheaper and Quality Medicines Act of 2008, pharmacists in the Philippines have a legal and ethical duty to promote the use of generic terminology and ensure patients are informed of the most affordable options. Advocacy in this context involves empowering the patient with information about bioequivalent generic alternatives and proactively communicating with prescribers when brand-only prescriptions create financial barriers that might lead to non-adherence, thereby upholding the patient’s right to health and access to essential drugs.
Incorrect: Focusing solely on internal pharmacy loyalty programs or discounts ignores the statutory requirement to offer generic alternatives which provide a more sustainable solution for medicine access. Attempting therapeutic substitution by switching to a different drug class without a new prescription or direct physician authorization is a violation of the Philippine Pharmacy Act (RA 10918) and exceeds the professional scope of a pharmacist. Delaying the provision of information about affordable government resources or generic options until after a high-cost sale is completed prioritizes commercial interests over the ethical obligation to facilitate immediate access to affordable care.
Takeaway: Pharmacists must actively offer generic alternatives and collaborate with prescribers to overcome financial barriers, ensuring compliance with Philippine laws that protect a patient’s right to affordable essential medicines.
Incorrect
Correct: Under Republic Act No. 6675, also known as the Generics Act of 1988, and Republic Act No. 9502, the Universally Accessible Cheaper and Quality Medicines Act of 2008, pharmacists in the Philippines have a legal and ethical duty to promote the use of generic terminology and ensure patients are informed of the most affordable options. Advocacy in this context involves empowering the patient with information about bioequivalent generic alternatives and proactively communicating with prescribers when brand-only prescriptions create financial barriers that might lead to non-adherence, thereby upholding the patient’s right to health and access to essential drugs.
Incorrect: Focusing solely on internal pharmacy loyalty programs or discounts ignores the statutory requirement to offer generic alternatives which provide a more sustainable solution for medicine access. Attempting therapeutic substitution by switching to a different drug class without a new prescription or direct physician authorization is a violation of the Philippine Pharmacy Act (RA 10918) and exceeds the professional scope of a pharmacist. Delaying the provision of information about affordable government resources or generic options until after a high-cost sale is completed prioritizes commercial interests over the ethical obligation to facilitate immediate access to affordable care.
Takeaway: Pharmacists must actively offer generic alternatives and collaborate with prescribers to overcome financial barriers, ensuring compliance with Philippine laws that protect a patient’s right to affordable essential medicines.
-
Question 14 of 29
14. Question
Operational review demonstrates that the electronic analytical balance used for weighing potent active pharmaceutical ingredients (APIs) has not undergone external certification for twelve months, although daily internal sensitivity checks are performed. According to Philippine FDA standards and Good Compounding Practices, what is the most appropriate action for the supervising pharmacist to take?
Correct
Correct: Suspend the use of the balance for potent substances until a third-party calibration service provider accredited by the National Metrology Laboratory or an equivalent body verifies its accuracy. This approach aligns with Philippine FDA Administrative Orders and the Philippine Pharmacy Act (RA 10918), which require that all instruments used in the compounding of drug products be calibrated at specific intervals to ensure accuracy and traceability. While internal checks are necessary for daily verification, they do not replace the legal and quality requirement for external certification by an accredited entity to guarantee the integrity of potent drug measurements.
Incorrect: Continuing operations based solely on internal sensitivity checks or automated software adjustments is insufficient because internal checks do not account for external environmental factors or mechanical wear that requires professional certification. Documenting the deviation in a logbook without taking corrective action to halt the use of the equipment fails to meet the safety standards of Good Compounding Practices, as it allows for the potential production of sub-potent or super-potent medications, which is a direct violation of the pharmacist’s duty to ensure patient safety.
Takeaway: Regulatory compliance in Philippine pharmacy practice requires that critical compounding equipment undergo periodic external calibration by accredited providers to ensure measurement traceability and dosage accuracy.
Incorrect
Correct: Suspend the use of the balance for potent substances until a third-party calibration service provider accredited by the National Metrology Laboratory or an equivalent body verifies its accuracy. This approach aligns with Philippine FDA Administrative Orders and the Philippine Pharmacy Act (RA 10918), which require that all instruments used in the compounding of drug products be calibrated at specific intervals to ensure accuracy and traceability. While internal checks are necessary for daily verification, they do not replace the legal and quality requirement for external certification by an accredited entity to guarantee the integrity of potent drug measurements.
Incorrect: Continuing operations based solely on internal sensitivity checks or automated software adjustments is insufficient because internal checks do not account for external environmental factors or mechanical wear that requires professional certification. Documenting the deviation in a logbook without taking corrective action to halt the use of the equipment fails to meet the safety standards of Good Compounding Practices, as it allows for the potential production of sub-potent or super-potent medications, which is a direct violation of the pharmacist’s duty to ensure patient safety.
Takeaway: Regulatory compliance in Philippine pharmacy practice requires that critical compounding equipment undergo periodic external calibration by accredited providers to ensure measurement traceability and dosage accuracy.
-
Question 15 of 29
15. Question
What factors determine the mandatory procedural response of a pharmacist in a Philippine community setting when a product is identified as a suspected counterfeit under the Special Law on Counterfeit Drugs (RA 8203)?
Correct
Correct: Under the Special Law on Counterfeit Drugs (Republic Act No. 8203) and the Food and Drug Administration (FDA) Act of 2009 (RA 9711), the pharmacist is legally obligated to immediately quarantine the suspected counterfeit products to prevent further distribution. The discovery must be reported to the FDA within the prescribed timeframe, and all relevant documents, such as invoices and delivery receipts, must be preserved to assist in the regulatory investigation and maintain the chain of custody.
Incorrect: Returning the suspected products to the distributor for a refund is incorrect because it allows potentially dangerous goods to re-enter the supply chain and may result in the destruction of evidence. Performing an independent chemical assay is not the responsibility of the retail pharmacist; forensic verification is the mandate of the FDA laboratories. Notifying only the manufacturer for a voluntary recall is insufficient because the pharmacist has a primary legal duty to report suspected criminal activity, such as counterfeiting, directly to the FDA as the lead enforcement agency.
Takeaway: In the Philippine regulatory framework, the discovery of counterfeit medicines requires immediate isolation of the stock and formal notification to the FDA to facilitate legal action and protect public health.
Incorrect
Correct: Under the Special Law on Counterfeit Drugs (Republic Act No. 8203) and the Food and Drug Administration (FDA) Act of 2009 (RA 9711), the pharmacist is legally obligated to immediately quarantine the suspected counterfeit products to prevent further distribution. The discovery must be reported to the FDA within the prescribed timeframe, and all relevant documents, such as invoices and delivery receipts, must be preserved to assist in the regulatory investigation and maintain the chain of custody.
Incorrect: Returning the suspected products to the distributor for a refund is incorrect because it allows potentially dangerous goods to re-enter the supply chain and may result in the destruction of evidence. Performing an independent chemical assay is not the responsibility of the retail pharmacist; forensic verification is the mandate of the FDA laboratories. Notifying only the manufacturer for a voluntary recall is insufficient because the pharmacist has a primary legal duty to report suspected criminal activity, such as counterfeiting, directly to the FDA as the lead enforcement agency.
Takeaway: In the Philippine regulatory framework, the discovery of counterfeit medicines requires immediate isolation of the stock and formal notification to the FDA to facilitate legal action and protect public health.
-
Question 16 of 29
16. Question
Consider a scenario where a supervising pharmacist in a community pharmacy in the Philippines is tasked with developing a new set of Key Performance Indicators (KPIs) for the pharmacy staff to ensure compliance with the Philippine Pharmacy Act (RA 10918) and the standards of Good Pharmacy Practice. From the perspective of the patient as a primary stakeholder, which approach to performance measurement best ensures that the pharmacist fulfills their legal and professional obligations?
Correct
Correct: Implementing a balanced scorecard that prioritizes the frequency and documented quality of patient counseling sessions and the accuracy of medication therapy reviews aligns with Republic Act No. 10918, also known as the Philippine Pharmacy Act. This law emphasizes the pharmacist’s role in providing patient-centered care and ensuring the safe and effective use of drugs. By measuring the quality of counseling and clinical reviews, the pharmacy ensures compliance with the mandatory requirement for pharmacists to be physically present to provide professional services, as stipulated in the standards of Good Pharmacy Practice (GPP) adopted by the Philippine FDA and the Professional Regulatory Board of Pharmacy.
Incorrect: Prioritizing the volume of prescriptions filled per hour or inventory turnover focuses on operational efficiency and commercial throughput, which may lead to the neglect of mandatory counseling and safety checks required under Philippine law. Evaluating staff based on their ability to consistently recommend complementary health supplements shifts the focus from clinical necessity to profit, potentially violating the ethical standards of the profession and the spirit of RA 10918. Using speed of dispensing as the primary metric for competence is insufficient because it does not account for the accuracy of the medication dispensed or the adequacy of the patient education provided, both of which are critical legal requirements for pharmacists in the Philippines.
Takeaway: Key Performance Indicators for pharmacy staff in the Philippines must prioritize clinical outcomes and patient safety over purely commercial or speed-related targets to remain compliant with the mandates of RA 10918.
Incorrect
Correct: Implementing a balanced scorecard that prioritizes the frequency and documented quality of patient counseling sessions and the accuracy of medication therapy reviews aligns with Republic Act No. 10918, also known as the Philippine Pharmacy Act. This law emphasizes the pharmacist’s role in providing patient-centered care and ensuring the safe and effective use of drugs. By measuring the quality of counseling and clinical reviews, the pharmacy ensures compliance with the mandatory requirement for pharmacists to be physically present to provide professional services, as stipulated in the standards of Good Pharmacy Practice (GPP) adopted by the Philippine FDA and the Professional Regulatory Board of Pharmacy.
Incorrect: Prioritizing the volume of prescriptions filled per hour or inventory turnover focuses on operational efficiency and commercial throughput, which may lead to the neglect of mandatory counseling and safety checks required under Philippine law. Evaluating staff based on their ability to consistently recommend complementary health supplements shifts the focus from clinical necessity to profit, potentially violating the ethical standards of the profession and the spirit of RA 10918. Using speed of dispensing as the primary metric for competence is insufficient because it does not account for the accuracy of the medication dispensed or the adequacy of the patient education provided, both of which are critical legal requirements for pharmacists in the Philippines.
Takeaway: Key Performance Indicators for pharmacy staff in the Philippines must prioritize clinical outcomes and patient safety over purely commercial or speed-related targets to remain compliant with the mandates of RA 10918.
-
Question 17 of 29
17. Question
The risk matrix shows that failure to properly record clinical activities significantly increases the likelihood of medication errors and legal liability for the healthcare facility. When a pharmacist identifies a significant drug-related problem and successfully collaborates with a physician to modify a patient’s therapy, which of the following documentation approaches best aligns with the Philippine Pharmacy Act and Good Pharmacy Practice standards?
Correct
Correct: Under Republic Act No. 10918, also known as the Philippine Pharmacy Act, and the Philippine Practice Standards for Pharmacists, documenting clinical interventions is a core professional responsibility. Recording the intervention in the official medical record ensures that all members of the healthcare team are informed of the clinical rationale and the agreed-upon plan, which is vital for continuity of care. Simultaneously, maintaining a pharmacy-specific clinical intervention log provides the necessary data for quality improvement and serves as legal evidence of the pharmacist’s professional actions and adherence to Good Pharmacy Practice (GPP) as mandated by the Food and Drug Administration (FDA).
Incorrect: Maintaining a private personal log while only updating the medication administration record is insufficient because it lacks the clinical justification for the change, which is necessary for other stakeholders to provide safe care. Documenting solely for administrative productivity metrics prioritizes institutional reporting over patient-centered clinical accountability and legal documentation requirements. Relying on the physician’s progress notes or verbal communication with nursing staff is a high-risk practice that fails to establish the pharmacist’s independent professional intervention, potentially leading to liability issues and gaps in the patient’s clinical history.
Takeaway: In Philippine pharmacy practice, clinical interventions must be documented in both the patient’s medical record and the pharmacy’s clinical log to satisfy legal requirements and ensure multidisciplinary patient safety.
Incorrect
Correct: Under Republic Act No. 10918, also known as the Philippine Pharmacy Act, and the Philippine Practice Standards for Pharmacists, documenting clinical interventions is a core professional responsibility. Recording the intervention in the official medical record ensures that all members of the healthcare team are informed of the clinical rationale and the agreed-upon plan, which is vital for continuity of care. Simultaneously, maintaining a pharmacy-specific clinical intervention log provides the necessary data for quality improvement and serves as legal evidence of the pharmacist’s professional actions and adherence to Good Pharmacy Practice (GPP) as mandated by the Food and Drug Administration (FDA).
Incorrect: Maintaining a private personal log while only updating the medication administration record is insufficient because it lacks the clinical justification for the change, which is necessary for other stakeholders to provide safe care. Documenting solely for administrative productivity metrics prioritizes institutional reporting over patient-centered clinical accountability and legal documentation requirements. Relying on the physician’s progress notes or verbal communication with nursing staff is a high-risk practice that fails to establish the pharmacist’s independent professional intervention, potentially leading to liability issues and gaps in the patient’s clinical history.
Takeaway: In Philippine pharmacy practice, clinical interventions must be documented in both the patient’s medical record and the pharmacy’s clinical log to satisfy legal requirements and ensure multidisciplinary patient safety.
-
Question 18 of 29
18. Question
Quality control measures reveal that a non-sterile oral aqueous suspension compounded in a community pharmacy lacks specific stability data from the manufacturer for its specific vehicle. According to the standards recognized by the Philippine Food and Drug Administration and the Philippine Pharmacy Act, how should the pharmacist determine the beyond-use date (BUD) for this preparation when stored at controlled cold temperatures?
Correct
Correct: Assigning a maximum BUD of 14 days for water-containing oral formulations stored at controlled cold temperatures is consistent with USP 795 standards, which are the recognized guidelines for compounding under the Philippine Pharmacy Act (RA 10918) and Philippine FDA regulations. This conservative approach accounts for the high risk of microbial growth and chemical degradation in aqueous environments when specific stability data is absent.
Incorrect: Assigning a 30-day BUD is incorrect because this timeframe is typically reserved for water-containing topical, mucosal, or dermal semi-solid formulations, not oral liquids. Using the manufacturer’s expiration date of the API is inappropriate because the stability of a compounded preparation is affected by the vehicle and environmental factors, not just the raw ingredient. Extending the BUD to 90 days based solely on the presence of a preservative is unsafe and violates standard compounding practices, as preservatives do not replace the need for stability testing for long-term dating.
Takeaway: In the absence of specific stability information, pharmacists must adhere to the conservative BUD limits for water-containing oral preparations to ensure patient safety and product integrity.
Incorrect
Correct: Assigning a maximum BUD of 14 days for water-containing oral formulations stored at controlled cold temperatures is consistent with USP 795 standards, which are the recognized guidelines for compounding under the Philippine Pharmacy Act (RA 10918) and Philippine FDA regulations. This conservative approach accounts for the high risk of microbial growth and chemical degradation in aqueous environments when specific stability data is absent.
Incorrect: Assigning a 30-day BUD is incorrect because this timeframe is typically reserved for water-containing topical, mucosal, or dermal semi-solid formulations, not oral liquids. Using the manufacturer’s expiration date of the API is inappropriate because the stability of a compounded preparation is affected by the vehicle and environmental factors, not just the raw ingredient. Extending the BUD to 90 days based solely on the presence of a preservative is unsafe and violates standard compounding practices, as preservatives do not replace the need for stability testing for long-term dating.
Takeaway: In the absence of specific stability information, pharmacists must adhere to the conservative BUD limits for water-containing oral preparations to ensure patient safety and product integrity.
-
Question 19 of 29
19. Question
Governance review demonstrates that a community pharmacy in a high-traffic urban area has experienced a five percent discrepancy in its inventory of Philippine Schedule IV substances over the last quarter. The current security protocol relies on a manual logbook and a single-lock cabinet managed by the pharmacist-on-duty. To enhance security measures and ensure compliance with the Department of Health and FDA regulations regarding the prevention of internal and external theft, which of the following strategies should the supervising pharmacist implement?
Correct
Correct: Implementing a dual-custodianship protocol for high-risk inventory access combined with biometric-linked electronic logging and regular unannounced inventory audits. This approach aligns with the Comprehensive Dangerous Drugs Act of 2002 (RA 9165) and the Philippine Pharmacy Act (RA 10918), which emphasize the pharmacist’s responsibility in maintaining the integrity of the supply chain. Dual-custodianship ensures that no single individual has unilateral access to sensitive stock, while biometric logging provides non-repudiable evidence of access, significantly reducing the risk of internal diversion and improving accountability during regulatory inspections by the Food and Drug Administration (FDA).
Incorrect: Increasing external security patrols and focusing CCTV primarily on customer service areas addresses external threats like shoplifting but fails to provide the necessary oversight for internal diversion, which is a major source of loss for regulated substances. Assigning a single senior pharmacist to manage all inventory keys creates a single point of failure and lacks the checks and balances provided by a multi-person verification system, potentially increasing the risk of coercion or internal theft. Utilizing a perpetual inventory system for automatic reordering is an operational efficiency measure for stock management rather than a security strategy designed to detect or prevent unauthorized removal of medications.
Takeaway: Comprehensive pharmacy security must integrate physical access controls, digital accountability, and procedural audits to mitigate both internal diversion and external theft in compliance with Philippine regulatory standards.
Incorrect
Correct: Implementing a dual-custodianship protocol for high-risk inventory access combined with biometric-linked electronic logging and regular unannounced inventory audits. This approach aligns with the Comprehensive Dangerous Drugs Act of 2002 (RA 9165) and the Philippine Pharmacy Act (RA 10918), which emphasize the pharmacist’s responsibility in maintaining the integrity of the supply chain. Dual-custodianship ensures that no single individual has unilateral access to sensitive stock, while biometric logging provides non-repudiable evidence of access, significantly reducing the risk of internal diversion and improving accountability during regulatory inspections by the Food and Drug Administration (FDA).
Incorrect: Increasing external security patrols and focusing CCTV primarily on customer service areas addresses external threats like shoplifting but fails to provide the necessary oversight for internal diversion, which is a major source of loss for regulated substances. Assigning a single senior pharmacist to manage all inventory keys creates a single point of failure and lacks the checks and balances provided by a multi-person verification system, potentially increasing the risk of coercion or internal theft. Utilizing a perpetual inventory system for automatic reordering is an operational efficiency measure for stock management rather than a security strategy designed to detect or prevent unauthorized removal of medications.
Takeaway: Comprehensive pharmacy security must integrate physical access controls, digital accountability, and procedural audits to mitigate both internal diversion and external theft in compliance with Philippine regulatory standards.
-
Question 20 of 29
20. Question
Benchmark analysis indicates that a supervising pharmacist at a community pharmacy in Manila has observed a colleague repeatedly dispensing prescription-only medications without valid prescriptions and failing to perform mandatory patient counseling on high-risk medications. Despite several informal discussions regarding these violations of Republic Act No. 10918, the colleague continues to exhibit these behaviors, which have led to documented near-miss medication errors. According to the Philippine regulatory framework and the Code of Ethics for Pharmacists, what is the most appropriate course of action for the supervising pharmacist?
Correct
Correct: Under Republic Act No. 10918, also known as the Philippine Pharmacy Act, and the Code of Ethics for Pharmacists in the Philippines, a pharmacist is mandated to uphold the highest standards of the profession and prioritize patient safety. When a colleague demonstrates persistent incompetence or unethical behavior that endangers public health, the pharmacist has a legal and ethical responsibility to document these occurrences and report the matter to the Professional Regulatory Board of Pharmacy. This formal reporting mechanism allows the Professional Regulation Commission to conduct a proper administrative investigation and implement necessary disciplinary actions, such as license suspension or revocation, to ensure that only competent individuals practice the profession.
Incorrect: Initiating a formal peer-review process for remedial training is a proactive management step, but it is insufficient when the colleague’s actions represent a significant breach of professional standards that requires regulatory oversight. Limiting a colleague’s duties to administrative tasks or implementing a probationary period addresses the immediate internal risk but fails to fulfill the statutory duty to report professional misconduct to the national regulatory body, potentially allowing the individual to continue practicing incompetently elsewhere. Requesting mediation through professional organizations like the Philippine Pharmacists Association is suitable for resolving ethical dilemmas or interpersonal conflicts but does not replace the legal requirement to report violations of the Philippine Pharmacy Act to the Board of Pharmacy.
Takeaway: Pharmacists in the Philippines are legally obligated to report incompetent or unethical colleagues to the Professional Regulatory Board of Pharmacy to protect public welfare and maintain professional integrity.
Incorrect
Correct: Under Republic Act No. 10918, also known as the Philippine Pharmacy Act, and the Code of Ethics for Pharmacists in the Philippines, a pharmacist is mandated to uphold the highest standards of the profession and prioritize patient safety. When a colleague demonstrates persistent incompetence or unethical behavior that endangers public health, the pharmacist has a legal and ethical responsibility to document these occurrences and report the matter to the Professional Regulatory Board of Pharmacy. This formal reporting mechanism allows the Professional Regulation Commission to conduct a proper administrative investigation and implement necessary disciplinary actions, such as license suspension or revocation, to ensure that only competent individuals practice the profession.
Incorrect: Initiating a formal peer-review process for remedial training is a proactive management step, but it is insufficient when the colleague’s actions represent a significant breach of professional standards that requires regulatory oversight. Limiting a colleague’s duties to administrative tasks or implementing a probationary period addresses the immediate internal risk but fails to fulfill the statutory duty to report professional misconduct to the national regulatory body, potentially allowing the individual to continue practicing incompetently elsewhere. Requesting mediation through professional organizations like the Philippine Pharmacists Association is suitable for resolving ethical dilemmas or interpersonal conflicts but does not replace the legal requirement to report violations of the Philippine Pharmacy Act to the Board of Pharmacy.
Takeaway: Pharmacists in the Philippines are legally obligated to report incompetent or unethical colleagues to the Professional Regulatory Board of Pharmacy to protect public welfare and maintain professional integrity.
-
Question 21 of 29
21. Question
Governance review demonstrates that a community pharmacy in Manila is planning to launch a marketing campaign for its new Medication Therapy Management (MTM) and immunization services. To ensure compliance with the Philippine Pharmacy Act (RA 10918) and the professional standards of the Professional Regulatory Board of Pharmacy, which approach should the supervising pharmacist adopt for the promotion of these professional services?
Correct
Correct: Highlighting the specific clinical qualifications of the pharmacist and the evidence-based health outcomes of the service in a professional manner. Under Republic Act No. 10918, also known as the Philippine Pharmacy Act, and the Code of Ethics for Pharmacists, any promotion of professional services must be dignified, truthful, and focused on the pharmacist’s role as a healthcare provider. This approach ensures that the public is informed of the value of the service without compromising the integrity of the profession or violating regulations regarding professional conduct.
Incorrect: Offering a limited-time discount on professional consultation fees to incentivize patient enrollment in a chronic disease management program is incorrect because discounting professional fees for clinical services can be viewed as unethical solicitation and devalues the professional judgment of the pharmacist. Using promotional materials that claim the pharmacy’s counseling services are superior to all other local providers based on internal satisfaction surveys is wrong because comparative advertising that claims superiority over other practitioners is generally discouraged and can be considered unprofessional conduct under the standards set by the Professional Regulatory Board of Pharmacy. Distributing brochures that promise a specific percentage improvement in blood glucose levels for all patients who complete the medication therapy management cycle is incorrect because guaranteeing specific clinical outcomes is prohibited as health results are multifactorial and such claims are considered misleading under FDA and PRBP regulations.
Takeaway: Professional pharmacy service promotion in the Philippines must be evidence-based and dignified, avoiding commercial gimmicks or guaranteed health outcomes that undermine professional ethics.
Incorrect
Correct: Highlighting the specific clinical qualifications of the pharmacist and the evidence-based health outcomes of the service in a professional manner. Under Republic Act No. 10918, also known as the Philippine Pharmacy Act, and the Code of Ethics for Pharmacists, any promotion of professional services must be dignified, truthful, and focused on the pharmacist’s role as a healthcare provider. This approach ensures that the public is informed of the value of the service without compromising the integrity of the profession or violating regulations regarding professional conduct.
Incorrect: Offering a limited-time discount on professional consultation fees to incentivize patient enrollment in a chronic disease management program is incorrect because discounting professional fees for clinical services can be viewed as unethical solicitation and devalues the professional judgment of the pharmacist. Using promotional materials that claim the pharmacy’s counseling services are superior to all other local providers based on internal satisfaction surveys is wrong because comparative advertising that claims superiority over other practitioners is generally discouraged and can be considered unprofessional conduct under the standards set by the Professional Regulatory Board of Pharmacy. Distributing brochures that promise a specific percentage improvement in blood glucose levels for all patients who complete the medication therapy management cycle is incorrect because guaranteeing specific clinical outcomes is prohibited as health results are multifactorial and such claims are considered misleading under FDA and PRBP regulations.
Takeaway: Professional pharmacy service promotion in the Philippines must be evidence-based and dignified, avoiding commercial gimmicks or guaranteed health outcomes that undermine professional ethics.
-
Question 22 of 29
22. Question
Governance review demonstrates that a local pharmaceutical laboratory in the Philippines has restructured its organizational chart so that the Quality Control (QC) Manager now reports to the Operations Director, who also oversees the Production Department. This change was intended to expedite the resolution of technical issues during the manufacturing process. According to the Current Good Manufacturing Practices (cGMP) guidelines adopted by the Philippine FDA, which action is necessary to ensure regulatory compliance regarding the independence of the Quality Unit?
Correct
Correct: Under the PIC/S Guide to Good Manufacturing Practice adopted by the Philippine FDA through Administrative Order No. 2012-0008, the Quality Control department must be independent from Production. This structural independence is fundamental to ensure that quality decisions, such as batch release or rejection, are not influenced by production pressures, deadlines, or output targets. Reporting to a director who also manages production creates a conflict of interest that compromises the integrity of the quality oversight.
Incorrect: Training the Operations Director in Quality Assurance does not resolve the structural conflict of interest inherent in overseeing both production and quality functions simultaneously. A consensus-based batch release protocol is insufficient because the Quality Unit must have the final, independent authority to reject materials or products without needing production’s agreement. Utilizing a third-party mediator is a temporary solution for conflict resolution but fails to address the permanent regulatory requirement for an independent organizational structure within the manufacturing facility.
Takeaway: The independence of the Quality Control unit from Production is a non-negotiable requirement of GMP to ensure unbiased assessment of product quality and safety.
Incorrect
Correct: Under the PIC/S Guide to Good Manufacturing Practice adopted by the Philippine FDA through Administrative Order No. 2012-0008, the Quality Control department must be independent from Production. This structural independence is fundamental to ensure that quality decisions, such as batch release or rejection, are not influenced by production pressures, deadlines, or output targets. Reporting to a director who also manages production creates a conflict of interest that compromises the integrity of the quality oversight.
Incorrect: Training the Operations Director in Quality Assurance does not resolve the structural conflict of interest inherent in overseeing both production and quality functions simultaneously. A consensus-based batch release protocol is insufficient because the Quality Unit must have the final, independent authority to reject materials or products without needing production’s agreement. Utilizing a third-party mediator is a temporary solution for conflict resolution but fails to address the permanent regulatory requirement for an independent organizational structure within the manufacturing facility.
Takeaway: The independence of the Quality Control unit from Production is a non-negotiable requirement of GMP to ensure unbiased assessment of product quality and safety.
-
Question 23 of 29
23. Question
Governance review demonstrates that the Pharmacy and Therapeutics Committee (PTC) of a tertiary government hospital is evaluating the inclusion of a novel, high-cost biological agent for the treatment of refractory rheumatoid arthritis. As the clinical pharmacist responsible for the formulary review, you are required to apply evidence-based medicine (EBM) principles in accordance with the Philippine Pharmacy Act (RA 10918) and the Department of Health (DOH) standards. Which of the following approaches best represents the correct application of EBM in this clinical decision-making process?
Correct
Correct: Systematically appraising the hierarchy of evidence, specifically focusing on high-quality randomized controlled trials and meta-analyses, is the cornerstone of evidence-based medicine. Under the Philippine Pharmacy Act (RA 10918), pharmacists are mandated to provide drug information and clinical services that are scientifically sound and evidence-based. Integrating this evidence with the patient’s specific clinical context and the Philippine healthcare setting, including alignment with the Philippine National Formulary (PNF) and Department of Health (DOH) standards, ensures both clinical efficacy and regulatory compliance.
Incorrect: Prioritizing clinical experience or manufacturer data alone fails to meet the standards of critical appraisal and may introduce significant bias into the decision-making process. Adhering strictly to international guidelines without local adaptation ignores the specific regulatory and economic constraints of the Philippine healthcare system and the requirements of the PNF. Relying solely on local retrospective observational data is insufficient for evaluating new therapies when higher-level evidence like meta-analyses is available, and it may delay necessary patient care or lead to suboptimal formulary decisions.
Takeaway: Clinical decision-making in pharmacy must balance the highest level of available scientific evidence with local regulatory standards and individual patient factors to ensure optimal and safe pharmacotherapy.
Incorrect
Correct: Systematically appraising the hierarchy of evidence, specifically focusing on high-quality randomized controlled trials and meta-analyses, is the cornerstone of evidence-based medicine. Under the Philippine Pharmacy Act (RA 10918), pharmacists are mandated to provide drug information and clinical services that are scientifically sound and evidence-based. Integrating this evidence with the patient’s specific clinical context and the Philippine healthcare setting, including alignment with the Philippine National Formulary (PNF) and Department of Health (DOH) standards, ensures both clinical efficacy and regulatory compliance.
Incorrect: Prioritizing clinical experience or manufacturer data alone fails to meet the standards of critical appraisal and may introduce significant bias into the decision-making process. Adhering strictly to international guidelines without local adaptation ignores the specific regulatory and economic constraints of the Philippine healthcare system and the requirements of the PNF. Relying solely on local retrospective observational data is insufficient for evaluating new therapies when higher-level evidence like meta-analyses is available, and it may delay necessary patient care or lead to suboptimal formulary decisions.
Takeaway: Clinical decision-making in pharmacy must balance the highest level of available scientific evidence with local regulatory standards and individual patient factors to ensure optimal and safe pharmacotherapy.
-
Question 24 of 29
24. Question
Governance review demonstrates that a community pharmacist in Quezon City is acting as a co-investigator for a Phase IV clinical trial involving a new oral hypoglycemic agent. During the recruitment phase, a regular patient who primarily speaks Tagalog and has limited formal education expresses interest in joining the study but appears confused by the technical terminology regarding pharmacokinetics and potential side effects listed in the English-language consent form. According to the Philippine Health Research Ethics Board (PHREB) guidelines and the Code of Ethics for Philippine Pharmacists, which action best ensures the ethical validity of the informed consent process?
Correct
Correct: The pharmacist must facilitate a comprehensive discussion in the participant’s preferred local dialect, utilize an impartial witness if literacy is an issue, and explicitly verify that the patient understands their participation is voluntary and entirely separate from their routine pharmaceutical care. This approach adheres to the Philippine Health Research Ethics Board (PHREB) guidelines, which emphasize that informed consent is a process of ensuring comprehension and protecting vulnerable subjects from therapeutic misconception, as well as the Data Privacy Act of 2012 (RA 10173) regarding the specific purpose of data collection.
Incorrect: Proceeding with enrollment based solely on a signed English-language form because it is the version approved by the ethics committee fails to meet the ethical requirement of ensuring the participant actually understands the risks and benefits. Offering preferential pharmacy services or priority access to medications as an incentive for participation constitutes undue inducement, which is prohibited under Philippine ethical standards for human protection. Delegating the entire explanation of the clinical trial to a pharmacy technician or non-pharmacist staff member is inappropriate, as the investigator or pharmacist holds the professional accountability to ensure the participant is fully informed about the pharmacological aspects and potential adverse reactions of the study.
Takeaway: In the Philippines, valid informed consent in pharmacy-based research requires the pharmacist to ensure the participant’s full comprehension through appropriate language and the absence of undue influence, regardless of the signed documentation.
Incorrect
Correct: The pharmacist must facilitate a comprehensive discussion in the participant’s preferred local dialect, utilize an impartial witness if literacy is an issue, and explicitly verify that the patient understands their participation is voluntary and entirely separate from their routine pharmaceutical care. This approach adheres to the Philippine Health Research Ethics Board (PHREB) guidelines, which emphasize that informed consent is a process of ensuring comprehension and protecting vulnerable subjects from therapeutic misconception, as well as the Data Privacy Act of 2012 (RA 10173) regarding the specific purpose of data collection.
Incorrect: Proceeding with enrollment based solely on a signed English-language form because it is the version approved by the ethics committee fails to meet the ethical requirement of ensuring the participant actually understands the risks and benefits. Offering preferential pharmacy services or priority access to medications as an incentive for participation constitutes undue inducement, which is prohibited under Philippine ethical standards for human protection. Delegating the entire explanation of the clinical trial to a pharmacy technician or non-pharmacist staff member is inappropriate, as the investigator or pharmacist holds the professional accountability to ensure the participant is fully informed about the pharmacological aspects and potential adverse reactions of the study.
Takeaway: In the Philippines, valid informed consent in pharmacy-based research requires the pharmacist to ensure the participant’s full comprehension through appropriate language and the absence of undue influence, regardless of the signed documentation.
-
Question 25 of 29
25. Question
The evaluation methodology shows that a pharmacist in a community setting is faced with an irate patient who claims that the generic medication dispensed during the previous visit was ineffective compared to the brand-name version. The patient demands an immediate refund and insists that the pharmacist should have ignored the generic dispensing requirement mandated by the Generics Act of 1988 (RA 6675). To mitigate professional risk and resolve the conflict while adhering to Philippine pharmacy regulations, what is the most appropriate course of action?
Correct
Correct: Acknowledging the patient’s concerns, explaining the bioequivalence standards enforced by the Philippine FDA, and documenting the suspected adverse drug reaction or therapeutic failure for reporting is the most appropriate action. This approach follows the professional standards set by the Philippine Pharmacy Act (RA 10918) and the Generics Act of 1988 (RA 6675), which require pharmacists to provide accurate information on generic medicines while fulfilling their role in pharmacovigilance. By documenting the incident, the pharmacist manages the risk of therapeutic failure while maintaining professional integrity and patient trust.
Incorrect: Offering an immediate exchange for the brand-name product at no cost is an inappropriate risk management strategy as it ignores the legal requirements of the Generics Act and creates a financial precedent that does not address the underlying clinical concern of bioequivalence. Referring the patient directly to the DOH regional office without attempting to resolve the issue or document the clinical complaint is a failure of the pharmacist’s duty to provide immediate patient care and professional counseling as mandated by the Code of Ethics for Philippine Pharmacists. Providing a partial refund and suggesting the physician prohibit generic substitution undermines the national policy of the Philippines to promote affordable quality medicines and fails to address the patient’s immediate dissatisfaction through proper education.
Takeaway: Conflict resolution in the Philippine pharmacy context must integrate patient empathy with a firm commitment to the Generics Act and the pharmacist’s responsibility to report suspected therapeutic failures to the FDA.
Incorrect
Correct: Acknowledging the patient’s concerns, explaining the bioequivalence standards enforced by the Philippine FDA, and documenting the suspected adverse drug reaction or therapeutic failure for reporting is the most appropriate action. This approach follows the professional standards set by the Philippine Pharmacy Act (RA 10918) and the Generics Act of 1988 (RA 6675), which require pharmacists to provide accurate information on generic medicines while fulfilling their role in pharmacovigilance. By documenting the incident, the pharmacist manages the risk of therapeutic failure while maintaining professional integrity and patient trust.
Incorrect: Offering an immediate exchange for the brand-name product at no cost is an inappropriate risk management strategy as it ignores the legal requirements of the Generics Act and creates a financial precedent that does not address the underlying clinical concern of bioequivalence. Referring the patient directly to the DOH regional office without attempting to resolve the issue or document the clinical complaint is a failure of the pharmacist’s duty to provide immediate patient care and professional counseling as mandated by the Code of Ethics for Philippine Pharmacists. Providing a partial refund and suggesting the physician prohibit generic substitution undermines the national policy of the Philippines to promote affordable quality medicines and fails to address the patient’s immediate dissatisfaction through proper education.
Takeaway: Conflict resolution in the Philippine pharmacy context must integrate patient empathy with a firm commitment to the Generics Act and the pharmacist’s responsibility to report suspected therapeutic failures to the FDA.
-
Question 26 of 29
26. Question
System analysis indicates that a community pharmacy has just received an official Class I recall notification from the Food and Drug Administration (FDA) Philippines regarding a widely dispensed antihypertensive medication found to contain a potent carcinogen. According to the Philippine Pharmacy Act and relevant FDA guidelines, which of the following represents the most appropriate professional procedure for the pharmacist to follow?
Correct
Correct: Under FDA Philippines Administrative Order No. 2016-0003 and Republic Act 10918, a Class I recall signifies a situation where there is a reasonable probability that the use of a product will cause serious adverse health consequences or death. The pharmacist is professionally and legally obligated to immediately isolate the affected stock in a dedicated quarantine area to prevent further dispensing. Furthermore, the pharmacist must proactively retrieve dispensing records to identify every patient who received the specific batch and contact them directly to ensure they cease use and return the product, as public safety takes precedence over administrative convenience.
Incorrect: Relying on the manufacturer or distributor representative to handle the patient notification process is inappropriate because the pharmacist holds the primary relationship and record of the patient, and any delay in notification increases the risk of harm. Posting general notices at the counter or on social media is an insufficient communication strategy for high-risk recalls where specific patients can be identified through pharmacy records. Simply returning the inventory to the distributor without attempting to reach patients who have already purchased the medication fails to address the ongoing risk to those individuals, violating the pharmacist’s duty of care under Philippine law.
Takeaway: For Class I recalls in the Philippines, pharmacists must execute immediate product quarantine and perform direct patient notification to mitigate life-threatening risks.
Incorrect
Correct: Under FDA Philippines Administrative Order No. 2016-0003 and Republic Act 10918, a Class I recall signifies a situation where there is a reasonable probability that the use of a product will cause serious adverse health consequences or death. The pharmacist is professionally and legally obligated to immediately isolate the affected stock in a dedicated quarantine area to prevent further dispensing. Furthermore, the pharmacist must proactively retrieve dispensing records to identify every patient who received the specific batch and contact them directly to ensure they cease use and return the product, as public safety takes precedence over administrative convenience.
Incorrect: Relying on the manufacturer or distributor representative to handle the patient notification process is inappropriate because the pharmacist holds the primary relationship and record of the patient, and any delay in notification increases the risk of harm. Posting general notices at the counter or on social media is an insufficient communication strategy for high-risk recalls where specific patients can be identified through pharmacy records. Simply returning the inventory to the distributor without attempting to reach patients who have already purchased the medication fails to address the ongoing risk to those individuals, violating the pharmacist’s duty of care under Philippine law.
Takeaway: For Class I recalls in the Philippines, pharmacists must execute immediate product quarantine and perform direct patient notification to mitigate life-threatening risks.
-
Question 27 of 29
27. Question
The efficiency study reveals that a pharmacy manager in a Philippine hospital setting needs to update the standard operating procedures for drug procurement to mitigate the risk of substandard medicines. According to the Philippine Pharmacy Act and FDA guidelines, which strategy should the pharmacist implement to ensure that only reputable suppliers are integrated into the supply chain?
Correct
Correct: Under Republic Act No. 10918, also known as the Philippine Pharmacy Act, and relevant FDA regulations, the pharmacist is the professional responsible for ensuring the quality, safety, and efficacy of pharmaceutical products. Implementing a mandatory verification protocol that requires a valid License to Operate (LTO) and a Certificate of Product Registration (CPR) for every item is the only way to ensure the supplier is legally authorized and the products are registered with the Philippine Food and Drug Administration. Cross-referencing these documents with the FDA verification portal is a critical best practice to prevent the entry of counterfeit or unregistered medicines into the pharmacy inventory.
Incorrect: Ranking suppliers primarily on fill rates focuses on logistical efficiency but fails to address the legal mandate of verifying product registration, which could lead to the procurement of unregistered items. Focusing on cost-containment and return policies prioritizes financial metrics over the pharmacist’s ethical and legal duty to guarantee drug safety through regulatory compliance. Selecting vendors based on geographical proximity and delivery speed addresses operational convenience but does not fulfill the regulatory necessity of ensuring the supplier holds a valid LTO and adheres to Good Distribution Practices.
Takeaway: The pharmacist must prioritize regulatory compliance by verifying the LTO and CPR of all suppliers to maintain the integrity of the pharmaceutical supply chain in the Philippines.
Incorrect
Correct: Under Republic Act No. 10918, also known as the Philippine Pharmacy Act, and relevant FDA regulations, the pharmacist is the professional responsible for ensuring the quality, safety, and efficacy of pharmaceutical products. Implementing a mandatory verification protocol that requires a valid License to Operate (LTO) and a Certificate of Product Registration (CPR) for every item is the only way to ensure the supplier is legally authorized and the products are registered with the Philippine Food and Drug Administration. Cross-referencing these documents with the FDA verification portal is a critical best practice to prevent the entry of counterfeit or unregistered medicines into the pharmacy inventory.
Incorrect: Ranking suppliers primarily on fill rates focuses on logistical efficiency but fails to address the legal mandate of verifying product registration, which could lead to the procurement of unregistered items. Focusing on cost-containment and return policies prioritizes financial metrics over the pharmacist’s ethical and legal duty to guarantee drug safety through regulatory compliance. Selecting vendors based on geographical proximity and delivery speed addresses operational convenience but does not fulfill the regulatory necessity of ensuring the supplier holds a valid LTO and adheres to Good Distribution Practices.
Takeaway: The pharmacist must prioritize regulatory compliance by verifying the LTO and CPR of all suppliers to maintain the integrity of the pharmaceutical supply chain in the Philippines.
-
Question 28 of 29
28. Question
System analysis indicates that a supervising pharmacist at a sterile compounding facility in Manila is updating the facilitys Standard Operating Procedures (SOPs) for environmental monitoring to align with Philippine FDA Administrative Order No. 2012-0008 and PIC/S GMP guidelines. To ensure the highest level of quality assurance and regulatory compliance for Grade A and B environments, which approach should the pharmacist prioritize for the viable environmental monitoring program?
Correct
Correct: Under the Philippine FDA Administrative Order No. 2012-0008, which adopts the PIC/S Guide to Good Manufacturing Practice, and USP 797 standards, environmental monitoring must reflect the environment during actual operational conditions. Performing volumetric air sampling and surface sampling during periods of peak activity, known as the dynamic state, ensures that the monitoring captures the highest potential microbial and particulate load. This approach provides a true assessment of the risk to sterile products during the compounding process.
Incorrect: Monitoring only during static conditions is insufficient because it fails to account for the primary source of contamination in cleanrooms, which is the personnel and their movements during actual work. Relying exclusively on settle plates is considered inadequate for high-risk areas like Grade A zones because they are passive sampling devices and do not provide a quantitative measure of a specific air volume, which is necessary for accurate microbial assessment. Setting alert levels based only on the maximum regulatory limits is a flawed approach because it ignores the requirement for trend analysis and the use of historical data to identify subtle deviations from the established baseline of a specific facility.
Takeaway: Effective environmental monitoring in sterile pharmacy practice must be conducted under dynamic conditions using quantitative methods to ensure compliance with PIC/S GMP standards as implemented by the Philippine FDA.
Incorrect
Correct: Under the Philippine FDA Administrative Order No. 2012-0008, which adopts the PIC/S Guide to Good Manufacturing Practice, and USP 797 standards, environmental monitoring must reflect the environment during actual operational conditions. Performing volumetric air sampling and surface sampling during periods of peak activity, known as the dynamic state, ensures that the monitoring captures the highest potential microbial and particulate load. This approach provides a true assessment of the risk to sterile products during the compounding process.
Incorrect: Monitoring only during static conditions is insufficient because it fails to account for the primary source of contamination in cleanrooms, which is the personnel and their movements during actual work. Relying exclusively on settle plates is considered inadequate for high-risk areas like Grade A zones because they are passive sampling devices and do not provide a quantitative measure of a specific air volume, which is necessary for accurate microbial assessment. Setting alert levels based only on the maximum regulatory limits is a flawed approach because it ignores the requirement for trend analysis and the use of historical data to identify subtle deviations from the established baseline of a specific facility.
Takeaway: Effective environmental monitoring in sterile pharmacy practice must be conducted under dynamic conditions using quantitative methods to ensure compliance with PIC/S GMP standards as implemented by the Philippine FDA.
-
Question 29 of 29
29. Question
Stakeholder feedback indicates that a significant number of patients with chronic conditions in the Philippines struggle with medication adherence due to the high cost of brand-name prescriptions. According to the Philippine Pharmacy Act (RA 10918) and the Universally Accessible Cheaper and Quality Medicines Act (RA 9502), which of the following actions demonstrates the most appropriate professional advocacy for patient rights and access to essential medicines?
Correct
Correct: Facilitate the selection of the most cost-effective generic equivalent while providing comprehensive counseling on therapeutic equivalence and the patient’s right to choose. This approach is mandated by the Universally Accessible Cheaper and Quality Medicines Act (RA 9502) and the Philippine Pharmacy Act (RA 10918), which require pharmacists to inform patients of generic alternatives to ensure affordability and therapeutic adherence while respecting patient autonomy.
Incorrect: Recommending a different therapeutic class based on pharmacy-led promotional discounts is inappropriate because therapeutic substitution requires physician intervention and should be based on clinical evidence rather than commercial promotions. Providing a partial fill of a brand-name medication without discussing generic options is a reactive measure that fails to address the long-term financial barriers to access and risks patient non-adherence. Prioritizing manufacturer-sponsored loyalty programs for brand-name drugs before discussing generic alternatives contradicts the legal priority in the Philippines to promote generics as the primary means of ensuring affordable healthcare for all citizens.
Takeaway: Pharmacists in the Philippines are legally and ethically bound to advocate for patient access by prioritizing the disclosure and provision of quality generic medicines.
Incorrect
Correct: Facilitate the selection of the most cost-effective generic equivalent while providing comprehensive counseling on therapeutic equivalence and the patient’s right to choose. This approach is mandated by the Universally Accessible Cheaper and Quality Medicines Act (RA 9502) and the Philippine Pharmacy Act (RA 10918), which require pharmacists to inform patients of generic alternatives to ensure affordability and therapeutic adherence while respecting patient autonomy.
Incorrect: Recommending a different therapeutic class based on pharmacy-led promotional discounts is inappropriate because therapeutic substitution requires physician intervention and should be based on clinical evidence rather than commercial promotions. Providing a partial fill of a brand-name medication without discussing generic options is a reactive measure that fails to address the long-term financial barriers to access and risks patient non-adherence. Prioritizing manufacturer-sponsored loyalty programs for brand-name drugs before discussing generic alternatives contradicts the legal priority in the Philippines to promote generics as the primary means of ensuring affordable healthcare for all citizens.
Takeaway: Pharmacists in the Philippines are legally and ethically bound to advocate for patient access by prioritizing the disclosure and provision of quality generic medicines.